09 Sep Freaking Fractures! 11 Common Types and How to Manage Them
Is a fractured bone the same as a broken bone?
Yes, these are exactly the same thing, sometimes we just like to sound fancy by calling these fractures, otherwise, we may be a little more casual and call it a broken bone. It seems as if this is just one of those things like “is it a muscle strain or tear” where a little bit of our culture has decided that at one point in time they became two different things. So, yes, a fracture is the same as a broken bone, don’t let anyone tell you otherwise.
How does a fracture typically occur?
How long is a piece of string? I’ve heard countless stories of how people have suffered a fracture in my time working as a physio. So let’s look at common fracture sites and how they usually occur.
Hand and Wrist
These pretty much fall into two categories. We have one group, the elderly who have a lower bone mineral density which increases their risk of suffering a fracture already, may suffer a small tumble and suffer a broken bone. The second group is the much younger, much more athletic, sporting population. This group will pretty much always have a story of falling from a tackle and falling directly onto their outstretched hand and the immediate onset of pain, or there may be a direct blow to the hand such as in a tackle.
Forearm
Forearm fractures are pretty similar to wrist and hand fractures in that a fall onto an outstretched hand is the most common mechanism of injury. There is a small incidence of people suffering them from a direct injury – there may be a common story in martial arts or contact sports such as rugby.
Ankle and Foot
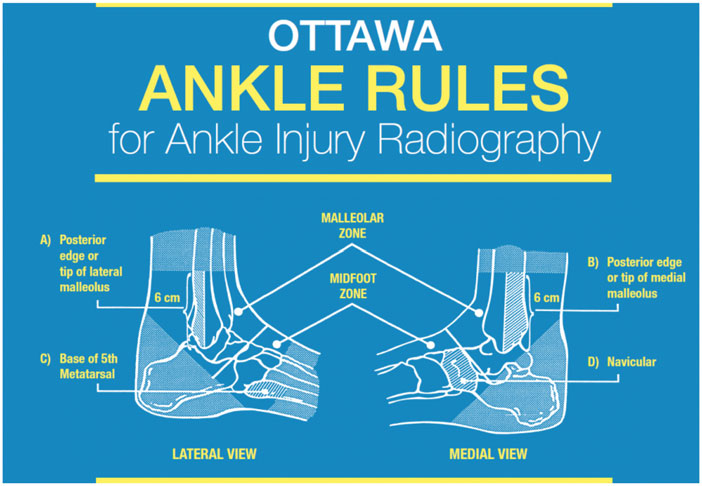
The ankle fractures are pretty classic, they usually occur in pretty much the same way we roll our ankles, they just require a little bit more force typically. Part of our routine assessments as physios is to utilise the Ottawa Ankle Rules to rule out the potential risk of a fracture. These tests aren’t specific but they are pretty good at picking up cases where there is a fracture. The most common mechanism would be an inversion ankle sprain where you can suffer a fracture of varying types around the lateral malleolus (outside ankle bone).
Other common fractures through the foot can be a Lisfranc fracture and fractures of the fifth metatarsal (which are really important to pick up!) Lisfranc fractures are most commonly sustained when you are twisting whilst falling down and can injure both bony structures as well as ligaments. In some cases, they may require surgical intervention to maximise the healing process and restore stability to the region. Fifth metatarsal fractures are another important fracture site to monitor as clinicians. They can occur either as acute injuries or as stress response injuries if you have suddenly increased your workload. Jones fractures are usually the worst one to get in the fifth metatarsal as it occurs in the area that has minimal blood flow so the risk of poor healing response is increased.
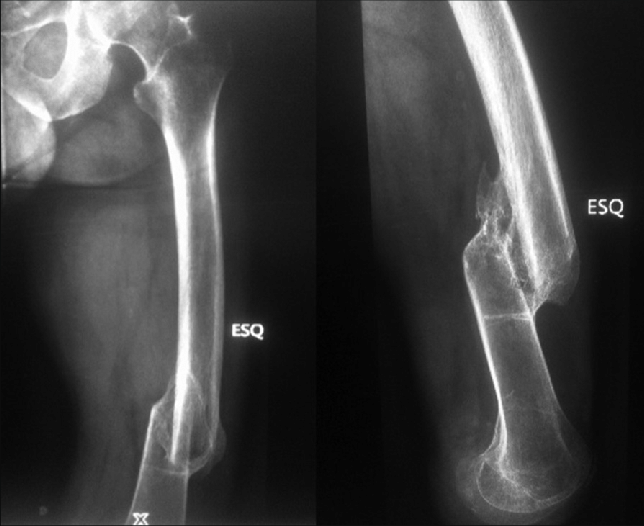
Shin
Shin fractures, with regards to acute fractures, are usually always due to a direct blow. Tibial stress fractures can occur but you will usually always have a lead-up of symptoms prior to the onset. Though I recall a case of a triathlete friend I had a few years ago who reported no shin pain, competed in a park run event on a Saturday morning and then was unable to weight bear that evening. A few days later we received her MRI and x-ray reports which showed that she had a significant tibial bone stress response and a stress fracture in her shin. This is not something that would have occurred within 24hrs and had been in the background for more than likely a few months. It’s always important to keep an eye out for odd little cases like these as clinicians.
Acute fractures can often occur with mechanisms such as a direct blow to the shin, an acute fall from a height or a twisting mechanism which can often present with a spiral fracture pattern. Tibial fractures are actually the most common long bone fracture, so if you suffer from one, you are far from alone!
How painful is a fractured bone?
Pretty bloody painful most of the time. It’s really not often I hear of many clients who suffer a fracture and don’t report a near on debilitating pain right from the second they felt it. Most fractures in the upper limb such as the wrist or the forearm are going to cause some pretty significant functional issues such as gripping, opening jars, and twisting door handles. Whereas lower limb fractures such as at the tibia, the ankle, or the foot usually are going to result in
What are the types of fractures?
A fracture is a fracture, isn’t it? Why do there have to be different types, imaging reports are already confusing enough with all of the medical words pumped in there let alone different types of fractures. Unfortunately, there are a lot of different types, and they can result in a lot of different treatment pathways. So let’s dig deep into them and discuss them all one by one to help you understand them.
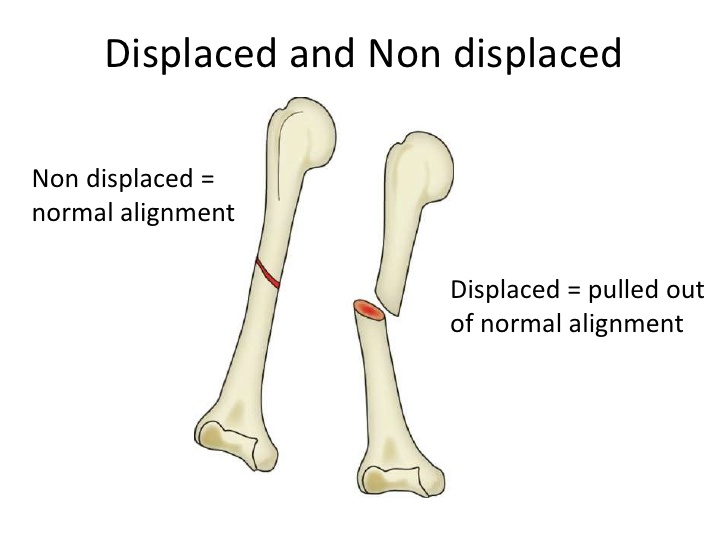
Displaced vs Non-displaced
A pretty simple distinction really, either the bone has been displaced and is “out of alignment” or it’s not. Probably the most common one I could think of for these would be a radius fracture in the forearm. I’m sure everyone has heard of someone who had a radius fracture and needed alignment while it was in a cast. Non-displaced fractures are much easier to manage, cast or offload and let the fracture healing process take place. Displaced fractures can be a little trickier. Those odd cases you hear of where someone had to have their bone rebroken? That’s probably a case of someone who had a displaced fracture that didn’t heal properly aligned.
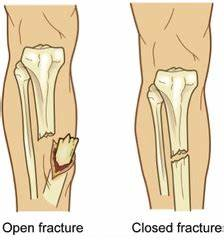
Open vs Closed
Again, another self-explanatory one, an open fracture occurs when there is a break in the skin, whereas a closed fracture is when there is no break in the skin. Open fractures are really important to manage well not just from a fracture perspective but also from a general health perspective. The risk of infection skyrockets in these cases particularly if you are on the sporting field. Getting appropriate management to manage the fracture to ensure proper fracture healing, but to also minimise the risk of infection is key. I would pretty much always be calling a paramedic in these cases.
Fracture Patterns
Avulsion Fracture
These occur when a fragment of the bone is pulled away from itself. A very common site for this is at the ankle following an inversion ankle sprain.
Buckled Fracture
This usually occurs when two ends of a bone are driven towards each other, it can also be referred to as an impacted fracture. It’s a common type of broken bone seen in young children.
Comminuted Fracture
These injuries are pretty well known, it’s those ones on the x-ray where it looks like the bone has shattered into many different pieces.
Compression/Wedge Fracture
Pretty common to see in the back after a fall or an impact-style injury. It can also be seen in older people with reduced bone mineral density after relatively innocuous injuries.
Greenstick Fracture
Can also be referred to as an incomplete fracture, it occurs when the bone is bent but not broken, again a relatively common injury to see in young children.
Linear Fracture
These injuries are diagnosed on the x-ray where the break occurs parallel to the bone’s long axis – for example, a radius fracture where the injury runs along the length of the radius rather than across it.
Oblique Fracture
Similarly diagnosed as a linear fracture but instead runs obliquely across the bone on a diagonal line.
Pathologic Fracture
These are injuries that are caused by an underlying pathological condition, common causes of these are cancer or osteoporosis.
Spiral Fracture
Spiral fractures occur where one portion of the bone has been twisted right at the point of injury.
Stress Fracture
These injuries occur after a prolonged period of bone stress, these don’t pop up quickly generally. They are usually small fractures surrounded by an area of bone under high stress.
Transverse Fracture
Essentially the exact opposite of linear fractures, rather than running along the long axis of the bone, runs perpendicular to the long axis of the bone.

Is a stress fracture and a normal fracture the same or are they different?
Whilst a true stress fracture, and not a stress response, requires a break within the bone, a stress fracture and a broken bone are two very different processes. A stress fracture develops over time – typically looking at weeks to months to develop. Clients will typically have experienced symptoms prior to the onset of the fracture as it developed as a stress response initially. Whereas, as we have discussed, a fracture is an acute break within the bone requiring a direct blow or direct force transfer through the bone in an instant resulting in a broken bone.
What is the normal healing time for a fracture?
There are a lot of factors that go into how long it takes for a fracture to heal. The healing process is largely dependent upon two factors – the age of the client, and the location of the fracture. Areas that have high levels of blood supply such as the spine and wrist will usually heal faster. This is compared to areas that have poor blood supply such as the fifth metatarsal, the scaphoid, or the tibia. Younger clients will typically have an accelerated healing process compared to older clients with some younger people being able to heal broken bones within 4 weeks, whereas in an older client this healing process could take 8 weeks. Of course, other factors such as the severity of the broken bone, length of time till management and how it was treated, as well as nutrition all impact how the healing process occurs.
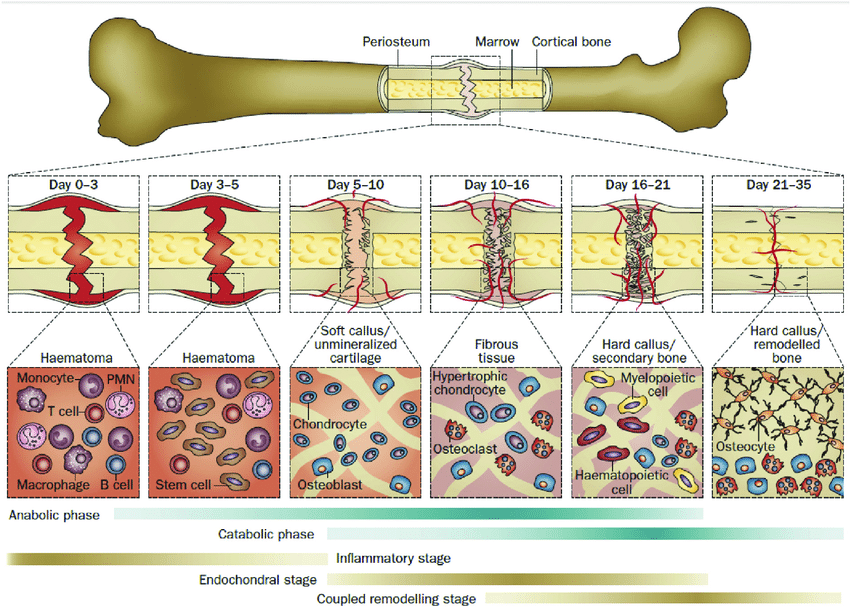
Stages of Fracture Healing
Haematoma Formation – Days 1 – 5
This process pretty much occurs between day one and day five and occurs immediately following the broken bone. When the fracture occurs, the blood vessels that supply the bone and the outer layer known as the periosteum are ruptured. This causes a hematoma to form at the fracture site, ultimately this hematoma will clot and form a frame around which the subsequent fracture healing can occur. The release of certain pro-inflammatory cytokines stimulates the gathering of macrophages, monocytes, and lymphocytes to the fracture. Together, these work to remove damaged, and necrotic tissue and release VEGF which to further stimulate healing.
Fibrocartilaginous callus formation – Days 5 to 11
The release of VEGF results in the development of fibrin-rich granulation tissue – fibrin is a non-globular protein involved in the clotting of blood, and granulation tissue is the connective tissue that forms on the outside of a wound. Mesenchymal stem cells are then recruited into the healing process, these differences between fibroblasts, chondroblasts, and osteoblasts. Together these work in a process called chondrogenesis – the development of cartilage, this forms the barrier spanning both ends of the fracture site. Whilst this is occurring, a layer of woven bone is laid down adjacent to the periosteal (outer) layers of the bone.
Bony callus formation – Days 11 to 28
Following that process, the callus of cartilage surrounding the fracture site begins to undergo a process called endochondral ossification. Essentially this is the process where chondroblasts, osteoblasts, and osteoclasts work together to resorb the callus and it begins to calcify and turn to bone. Deeper within the bone structure, woven bone continues to be laid down, and newly formed blood vessels are developed which allows for the further migration of stem cells within the bone structure. At the conclusion of this phase, there is a hard, calcified callus of immature bone where there was previously a broken bone.
Bone remodelling and addition of compact bone – Day 18 and onwards (months to years)
Eventually, this callus needs to be replaced by compact bone, this process is driven by osteoclasts and osteoblasts that remodel the bone via a process called coupled remodelling. The centre of the callus is replaced by compact bone, meanwhile, the callus edges are replaced by lamellar bone. Blood vessels continue to undergo changes at the same time. Ultimately this process takes time, months to years depending upon the person, but ultimately it results in the regeneration of a normal bone structure.
First aid for fractures
Think someone you know has a fracture? Dealing with it at the start will hopefully reduce any chance of preventing the break from getting worse either in size or altering its position and putting it in a misaligned position. Ideally, you want to offload and immobilise the potentially fractured site. If you are dealing with a lower limb fracture using crutches or a wheelchair to take the weight off is your best option. If it’s an upper limb fracture, using a sling can be a handy option, or if one isn’t readily available just using a shirt as a makeshift sling can work as well.
If it’s an open fracture try to keep the area as clean as possible and consider whether you need the assistance of paramedics to properly manage the injury.
Lastly, get imaging done as soon as possible to rule in or rule out a fracture and determine your best pathway for management. If you don’t know what you are dealing with, determining whether surgical input is needed to stabilise the broken bones is pretty hard, you may as well throw a dart at a dartboard while blindfolded after being spun around for 10 minutes.
Diagnosing a fracture
As physiotherapists, we are quite adept at picking up potential cases of ankle fractures utilising the Ottawa Ankle Rules. These rules help us identify clients who have an elevated risk of having sustained an ankle fracture. We are able to refer for ankle x-rays to determine whether a fracture is present or not. Ultimately x-ray is the best first step imaging process to go through. Some cases may require CT imaging but it is unlikely. MRI may be utilised in cases of clients with a stress fracture to determine whether there is a continuing bone stress response.
Complications of bone fractures
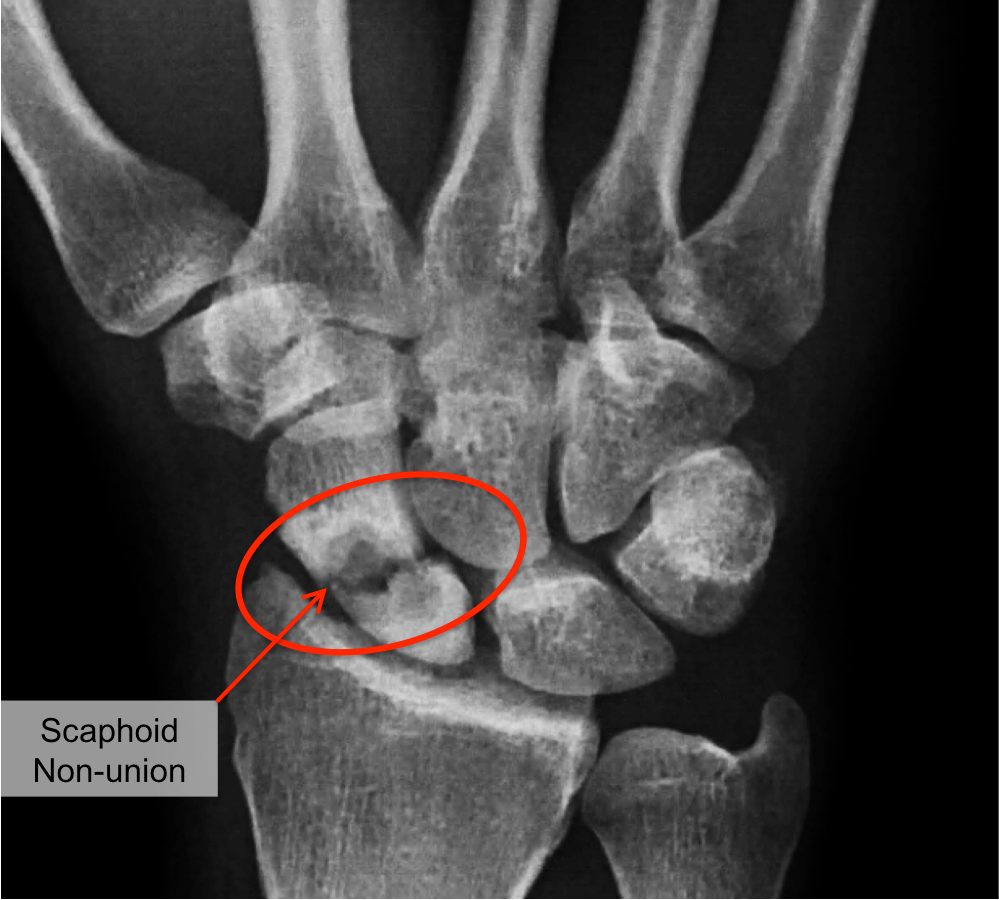
Non-union/Malunion
By far probably the most common complication in fracture management. While it is far from the end of the world, it does lengthen the management time for these injuries. It’s really important that you follow the restrictions put in place by the doctor who put the cast on or put the internal or external fixation in place. If you don’t follow the restrictions, the risk of nonunion or malunion increases. Nobody wants to be in a cast for twice as long, so it’s probably wise to just follow the instructions the first time around.
Infection
Infections are at a greater risk of happening in open fractures. Infection requires medical management usually through the use of antibiotics. It may potentially have a small impact on the fracture healing time, but will generally just not be a fun time dealing with a broken bone and an infection at the same time because they kinda suck enough on their own.
Neurovascular damage
It’s important that we don’t just focus all of our time and attention on the fracture if there are other things going on. If you experience numbness, sensation changes, or really cold extremities like toes and fingers, the risk of neural or vascular damage is there. It’s incredibly important you mention these symptoms to your therapist or doctor so that they can undertake any appropriate imaging or diagnostic steps.
DVT/Pulmonary Embolism
Blood clots can be one of the more common complications post-fracture, particularly if you take the rest part of RICE a little bit too seriously. Typically these will develop if you are inactive for long periods of time and don’t promote good blood flow. In some cases, there may be predisposing risk factors such as a history of cardiac issues, or overweight and previously sedentary people.
Avascular Necrosis
Necrosis is the process of death of tissue, the rates of avascular necrosis within fractures are pretty low but the consequences are pretty high. These are things to watch for in higher-risk fractures such as the scaphoid and the fifth metatarsal where there are lower rates of blood supply. Early identification through an x-ray or CT scan is important to ensure appropriate management from the outset.
What is the benefit of casting or booting a fracture?
Utilising casts and boots are ways that we work to reduce the load being transferred to the fracture site and immobilise the area. Casts are utilised most commonly for upper limb fractures, and boots can be utilised for certain ankle and foot fractures. Boots are a great option because they can allow people to still weight bear with the boot taking some of the load away. Casts simply immobilise the area and reduce your risk of malunion or non-union. These are great options for management, and if your doctor or physio recommends one I wouldn’t be skimping out on it.
Self Management of Fractures
This is not a section on how you should manage your fracture yourself just an FYI. Always get it seen by a health professional and I’d always recommend seeing a physio for hands-on treatment and exercise progressions and clearance for return to sport. What this section is about is what you can do at home to help yourself while you wait for the fracture healing process to take place.
Strengthening
Keeping up strength around the fracture is key. There’s nothing worse than coming out of a moon boot or a cast and having weeks and weeks of strengthening work to do to catch up. Keeping the other leg strong in cases of ankle or lower limb fractures as well as either above or below the site of the fracture on the same side. There’s a significant amount of research that shows if you keep exercising the opposite side of the body at the gym you minimise muscle loss on the fractured side. So keep in the gym and keep working.
For those of you with upper limb fractures, it may be a little harder. If you can keep your hand working by using theraputty bonus points. Theraputty is great for maintaining strength and dexterity through the hand and fingers, it is a very versatile exercise tool that you can utilise to strengthen anything ranging from pinching all the way to gripping. Otherwise keeping shoulder strength and mobility, as well as mobility around the elbow and wrist depending upon the fracture site is important too.
Stretches
Maintaining your range of motion is pretty critical in avoiding any restrictions coming out of your cast. Keeping as much mobility above and below the fracture site will put you in good stead. Suffered an ankle fracture? Keep your knee and hip range of motion as good as possible as well as your ankle mobility on the opposite side. If you’ve had an upper limb fracture keeping mobility in your hand, wrist, elbow, and shoulder as much as you can will help you rehab once you come back out of the cast.
Balance and Proprioception
Particularly important for those of you out there with lower limb fractures. Balance is one of the first few things to usually go and look at how some of these injuries happen, rehabbing it is vital. On the leg you are still able to weight bear on practising single leg balance with a variety of changes such as eyes closed, throwing a ball, mental challenges like maths, or reaching outside your centre of balance are great ways to keep your balance system improving.
What helps speed up bone healing rates?
Good nutrition
High-quality nutrition is pretty important for everything apparently. Good wholesome food helps maintain good levels of vitamins, nutrients, minerals etc that Maccas, KFC, or Red Rooster simply don’t give us. Make sure you stay on top of your nutrition game while you are off to keep off those extra few kilos but to also help out your fracture.
Dietary supplements
Certain supplements such as protein, calcium, vitamin D and vitamin C have some evidence that they can assist in fracture healing. I’m far from recommending you go racing out to go get them all and expect to be healed in a week, these are ways that assist your body in its healing process and allow the rest of your body to continue to function optimally.
What slows bone healing rates?
Smoking
Smoking doesn’t just affect your lungs, it also has effects on bone mineral density. Smokers have shown that they have lower levels of bone mineral density, as a result, this means not only are you at a heightened risk of sustaining a fracture, but it also impacts your body’s capacity to perform wound and injury healing.
Anemia
Anemia is essentially a lower level of red blood cells, it turns out these are pretty darn important for healing! A lower level of red blood cells simply means that the normal rate at which everything is typically transported is reduced a little bit. It won’t mean that your broken bones won’t heal or anything along those lines, it might just take a little bit longer.
What is the long-term outlook after a fracture?
Generally pretty good, the body is incredibly efficient at healing broken bones. Depending upon the type of fracture and the location of the fracture, a vast majority of clients are able to return to their previous way of life without worry in the world. In some cases that may struggle you will often be looking at people who have sustained multiple bone fractures, or complex fractures. Other complications such as infection delaying and interrupting bone healing could have potential longer-term impacts upon recovery. For other clients who require internal fixation of a fracture, there may potentially be some restrictions simply due to either pain from the fixation site, or from potential range of motion restrictions that the fixation causes.
Returning to sport after a fracture
Usually return to sport is pretty well uninhibited outside of the restrictions of fracture healing time. Once the healing process is complete and the fracture has united it is simply a matter of whether the athlete is fit enough to return to sport and whether they have completed the requisite amount of load to not risk other injuries. In pretty much any case of upper limb fractures staying mobile with running and training but with restrictions is the best way to keep your training load up while waiting for healing. For those who suffered a broken bone in their leg, it can get a little tougher, staying running while non-weight bearing is pretty hard. For these cases, it’s a matter of rebuilding the training load once they are cleared to return to sport.
Other Recent Posts
- Lifting Technique “Never Lift with a Bent Back” – Why Those Words Make me Shudder
- When should I see a Physio?
- Adductor Strains – A Footballers Worst Nightmare
- Hamstring Strains – Frustrating, Recurrent, Our process for how we can help you
- Gluteal Tendinopathy – It’s a Real Pain in the Ass
How Can We Help?
